TL;DR
- Laparoscopic surgery preserves ovarian function — small “keyhole” incisions allow cyst removal while minimising tissue loss, reducing adhesions, and supporting fertility.
- Fertility outcomes are generally positive — many women conceive within months to years after surgery, but success depends on ovarian reserve, cyst type, and overall reproductive health.
For many women, the path to pregnancy is already filled with challenges. When ovarian cysts enter the picture, the uncertainty can feel even greater: Will they affect your fertility? Do they always need surgery? And if surgery is recommended, will it help or harm your chances of conceiving?
Laparoscopic surgery — a minimally invasive “keyhole” technique — is often used to remove ovarian cysts while protecting the ovaries’ delicate structures. Done carefully, it can relieve symptoms, prevent complications, and even improve fertility outcomes.
This article explores how different types of ovarian cysts impact conception, the role of laparoscopic surgery in preserving ovarian function, and what you should know before deciding if this treatment is right for you.
What Are Ovarian Cysts?
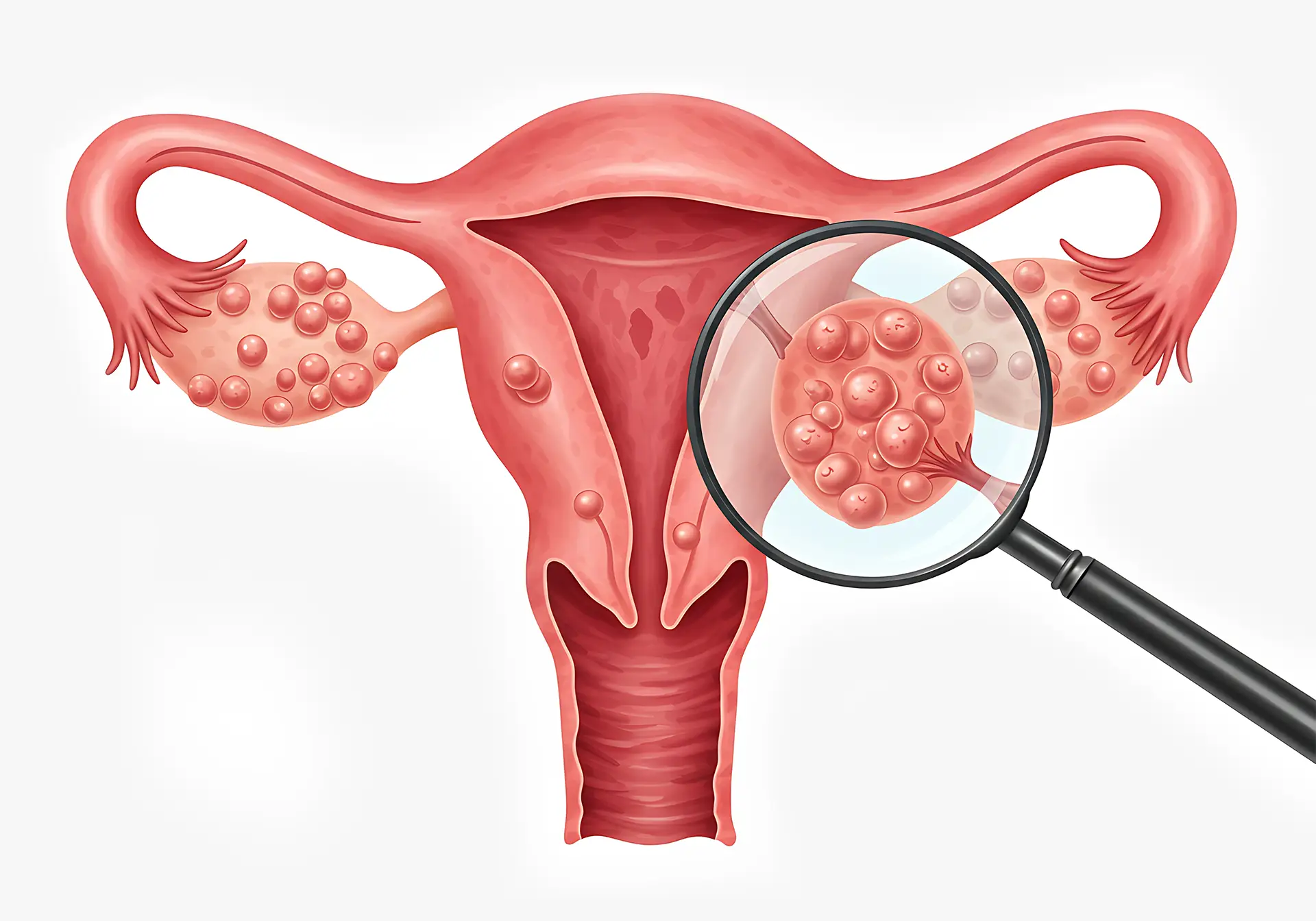
Ovarian cysts are fluid-filled sacs that develop on or inside the ovary. They’re common in women of reproductive age, and most disappear on their own without treatment. However, certain types of cysts can interfere with fertility, cause pain, or require surgical removal.
Types of Cysts That Impact Conception (Endometriomas, Dermoid, Cystadenomas)
1
Endometriomas
These cysts develop when endometrial tissue (the lining that grows inside the uterus) forms on the ovaries. Endometriomas are linked with endometriosis, a condition that can cause painful periods, damage healthy ovarian tissue, and affect egg quality.
2
Dermoid Cysts
3
Cystadenomas
These cysts form from the cells on the outer surface of the ovary. They can be filled with watery or mucous material. While not always harmful, larger cystadenomas may distort the ovary and affect nearby reproductive structures.
How Do Ovarian Cysts Affect Fertility?
Getting pregnant may be harder when cysts are persistent, large, or linked to endometriosis.
- Endometriomas in particular can damage the surrounding ovarian tissue, reducing the number of healthy eggs you have left.
- Larger cysts can physically change the shape of the ovary or press on nearby structures like the fallopian tubes. This can make it more difficult for eggs to be released, fertilised, or transported to the uterus.
- Some cysts disrupt the way your ovaries regulate hormones, interfering with ovulation — meaning eggs are not released regularly.
- Chronic pelvic pain from cysts or endometriosis may not directly prevent pregnancy, but it can complicate timing conception and make intercourse uncomfortable.
Role of Laparoscopic Surgery in Fertility Treatment
Many gynaecologists today recommend laparoscopic surgery, also known as “keyhole surgery”, to remove ovarian cysts in women who want to preserve or improve their fertility.
It involves making small incisions in the abdomen and using a thin camera with special instruments to access the ovaries. Compared with laparotomy (open surgery), it’s generally associated with:
- Quicker recovery, as most women experience less pain after surgery, spend less time in the hospital, and get back to their regular routine sooner.
- Less scar tissue (adhesions) left behind that might interfere with the fallopian tubes or uterus.
How the Procedure Preserves Ovarian Tissue and Function
Under the magnified view of the laparoscope, your surgeon removes the cyst wall from the ovary while leaving the surrounding healthy tissue in place. Instead of draining the fluid, your surgeon takes out the entire capsule, lowering the risk of recurrence.
Your surgeon also avoids disrupting the ovarian blood vessels, which are essential for blood flow, hormone production, and egg release.
By combining these steps, laparoscopic surgery treats the cyst while conserving as much ovarian tissue and function as possible.
Fertility Outcomes After Laparoscopic Cyst Removal
Laparoscopic surgery generally leads to strong fertility outcomes due to all the reasons stated above. Studies have found that 30% to 67% of women conceive in the first year post-surgery, and up to 64.4% within five years.
Laparoscopic surgery can improve your chances of pregnancy, but outcomes vary based on a person’s health profile. Need an assessment? Schedule an appointment with Dr Chang.
Preparing for Laparoscopic Surgery When Trying to Conceive
Before deciding on surgery, it’s important to assess both your ovarian reserve and your partner’s sperm health. Together, these tests give you a clearer picture of fertility and help your doctor plan the most appropriate treatment.
Pre-Surgical Fertility Tests (AMH, AFC, Partner’s Sperm Analysis)
- Anti-Müllerian Hormone (AMH): This blood test estimates your ovarian reserve. A lower AMH may mean fewer eggs, which could affect your chances of conception after surgery.
- Antral Follicle Count (AFC): Done via ultrasound, this test counts the small follicles in your ovaries. Together with AMH, it gives a clearer picture of egg supply.
- Semen Analysis: Knowing your partner’s sperm health is just as important. Testing motility, count, and morphology helps identify whether male factor infertility could also affect your fertility.
Questions to Ask Your Gynaecologist or Fertility Specialist
Fertility can be a sensitive subject and it can sometimes be hard to prepare questions ahead of your doctor’s visit. Here are some you can start with:
- How will this procedure affect my ovarian reserve?
- What are the chances of natural conception after surgery in my case?
- Should I consider egg freezing or in vitro fertilisation (IVF) before or after the procedure?
- How long should I wait before trying to conceive?
- What risks should I be aware of, and how are they managed?
After Surgery
Once your surgery is complete, recovery is usually straightforward. You may stay in the hospital for one or two nights before going home. Plan to rest during the first week, then slowly return to normal activities as you feel stronger.
Most doctors recommend waiting about three months before trying for pregnancy, to allow your ovaries time to heal fully. Your menstrual cycle usually resumes within one to two months.
Cost and Insurance Coverage in Singapore
Cost of Laparoscopic Ovarian Cystectomy With Fertility Considerations
Surgery fees can vary, and additional costs may come from fertility assessments such as hormone tests, ultrasound scans, and semen analysis.
Medisave and IVF-Related Coverage
For most women, laparoscopic ovarian cyst removal is considered medically necessary — especially if the cyst is painful, large, or could affect fertility. This means you can use Medisave to cover part of the bill, within limits set by the Ministry of Health (MOH).
You may also be able to claim from insurance, depending on your policy, but coverage generally doesn’t extend if the surgery is done purely for fertility reasons without other medical indications.
If your surgeon later recommends IVF, you may qualify for government co-funding at approved centres. The subsidies apply to the treatment itself, not the cyst removal.
Why It’s Important to Choose the Right Gynaecologist for Laparoscopic Surgery
When fertility is part of your plan, the way your cyst is removed matters as much as the decision to have surgery.
With over 25 years of experience in treating ovarian cysts and fertility-related conditions, Dr TC Chang offers personalised care that balances surgical precision with fertility planning.
Book a consultation with him today