Navigating a high-risk pregnancy can be worrisome, filled with uncertainties about your health and your baby’s well-being. To be better informed about your pregnancy, asking the right questions is essential.
Here are six crucial questions to ask your doctor and why they are important.
Why am I diagnosed with a high-risk pregnancy?
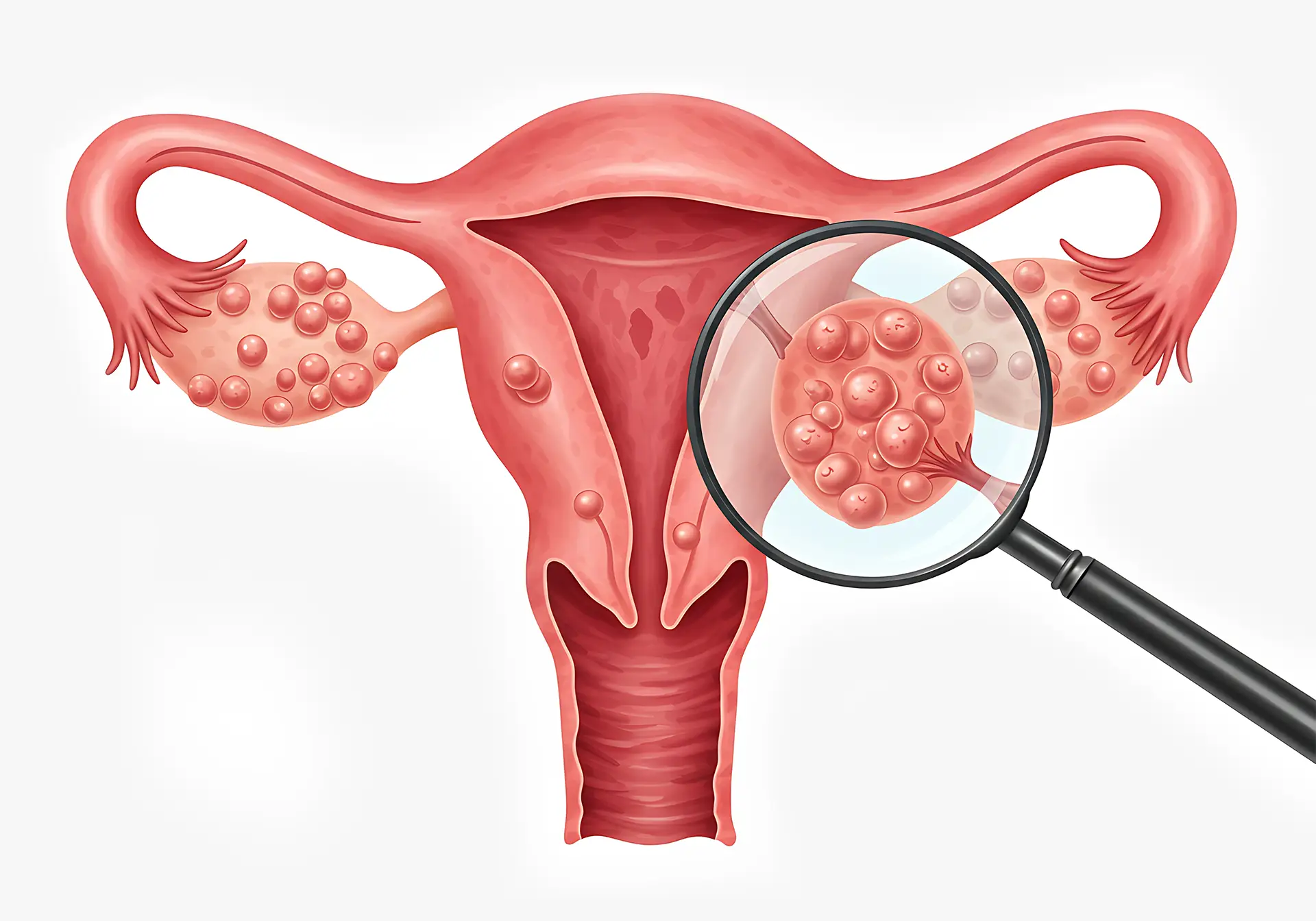
High-risk pregnancies can arise due to preexisting medical conditions, complications that develop during pregnancy, or lifestyle factors. Ask your doctor to explain the specific reasons for your diagnosis. This could include conditions such as hypertension, diabetes, heart disease, or autoimmune disorders.
Pregnancy-related issues like preeclampsia, gestational diabetes, multiple pregnancies (twins, triplets, etc.), or a history of complications in previous pregnancies are also contributing factors.
Understanding the underlying reasons helps you and your high-risk pregnancy doctor to tailor your care plan effectively. It also enables you to make informed decisions about your health and lifestyle adjustments to minimise risks.
What symptoms should I look out for?
Your obstetrician can provide a list of symptoms specific to high-risk pregnancies that you should monitor. Common symptoms to be aware of might include intense headaches, sudden swelling of the hands and face, vision changes, and intense upper abdominal pain, which can be signs of preeclampsia. Persistent back pain, regular contractions, or fluid leakage might indicate preterm labour.
Identifying these warning signs ensures you can seek prompt medical attention, potentially preventing more severe complications.
Can I carry my baby to full-term?
Preterm birth is a significant risk in high-risk pregnancies, and understanding your chances of carrying to full-term is vital for preparation and planning. Find out from your obstetrician the specific risks associated with your condition and the likelihood of preterm delivery.
Your obstetrician can explain the measures that can be taken to prolong your pregnancy safely, such as medications to prevent preterm labour, lifestyle adjustments, and bed rest if necessary.
Being aware allows you to plan for different scenarios and ensures that you are prepared for the possibility of an early delivery. It also allows you to discuss and arrange for neonatal care if required.
Is normal delivery possible with a high-risk pregnancy?
The possibility of a vaginal delivery largely depends on the specific risks and complications associated with your high-risk pregnancy. Check with your specialist about the feasibility of a normal delivery in your case.
The position and health of the baby, your health and medical history, and the presence of any complications such as placenta previa or preeclampsia are all factors that influence this decision. Your gynae will assess them throughout pregnancy to determine the safest delivery method.
In many cases, a vaginal delivery may still be possible with careful monitoring and appropriate interventions. However, it’s essential to remain flexible and prepared for the possibility of a caesarean section if complications arise during labour.
What can I do to minimise my risk?
Ask your gynae about specific actions you can take to reduce potential complications. This might include dietary recommendations to ensure you are getting the right nutrients, safe exercise routines to maintain your health without putting the pregnancy at risk, and guidelines on avoiding harmful substances like alcohol and tobacco.
Your doctor can also advise on managing stress and mental health, as emotional well-being is vital to high-risk pregnancy health. Medications might be necessary to control preexisting conditions or manage pregnancy-related issues.
How will this affect my prenatal and pregnancy care?
High-risk pregnancies often require a more intensive prenatal care regimen, including more frequent visits to the obstetrician and additional tests. Discuss with your gynae the frequency of your prenatal visits and what additional monitoring or tests will be necessary. These tests might include more frequent ultrasounds, non-stress tests, or specialised blood tests to monitor your and your baby’s health.
Anticipating these changes helps you prepare for the time commitment and potential logistical arrangements, such as arranging transportation or time off work. It also ensures that you know the resources available, such as support groups or counselling services.
Why should I be aware of these critical concerns?
Dealing with a high-risk pregnancy can indeed feel like an emotional rollercoaster, but being informed and proactive can make a significant difference. By asking the right questions and understanding your condition, you can better prepare for the journey.
Awareness also reduces anxiety and helps you feel more in control of your pregnancy journey. It allows you to communicate effectively with your high-risk pregnancy specialist and advocate for your and your baby’s needs.
Remember, you are not alone—your healthcare team is there to guide and support you every step of the way. Be informed, seek support, and focus on what you can control to create the best possible outcome for you and your baby.
High-risk Pregnancy Obstetrician in Singapore
If you are going through a high-risk pregnancy, having a skilled and experienced obstetrician is crucial. Dr T C Chang, an obstetrician in Singapore, has been managing patients with high-risk pregnancies for the last 26 years. Dr. Chang provides personalised care tailored to each patient’s unique needs.
His clinic offers comprehensive services, including advanced prenatal testing, close monitoring of both mother and baby and a supportive environment to address all your concerns. With a focus on evidence-based practices, Dr. Chang ensures that you receive care you need throughout your pregnancy.